INTRODUCTION:
The Discovery of penicillin was a great revolutionary event in the history of Medicine. The 1950s was known as the golden era. However, the evolution of antimicrobial resistance has posed as a global threat and this has become an issue of serious concern. Now we are heading towards the post-antibiotic era. According to WHO, small injuries may result in death in future, if we fail to act against antimicrobial resistance now Also, they predict that the human and animals may face Multi-Drug Resistance (MDR) epidemics as we faced cholera and tuberculosis epidemics in the past. The global antimicrobial resistance surveillance system reported that around 5,00,000 people are suffering from antimicrobial resistance annually. In the USA and Europe, nearly 50,000 people are dying each year due to antimicrobial resistance. In India, almost 60,000 newborn babies die every year due to infections caused by MDR bacteria. Director-General of WHO, Dr. Tedros Adhanom Ghebreyesus says, “Antimicrobial resistance is a global emergency that will seriously threaten in modern medicine”.
Antibiotics are also known as antibacterial agents, which were extensively used in the second half of the twentieth century. But after a few decades, the development of resistance in bacteria stopped their success as effective therapeutics. Humans have overused antibiotics for all kinds of simple bacterial infections, sore throat, and pneumonia. Antibiotics are not a treatment of choice for viral infections, but their use in common cold and simple viral disease is one of the most common factors responsible for the development of resistance. Infusion of a large number of antibiotics in agriculture, fisheries, animals, and food industries is a threat to the development and spread of AMR in human and animal pathogens as per CDC (Center for Disease Control and Prevention).
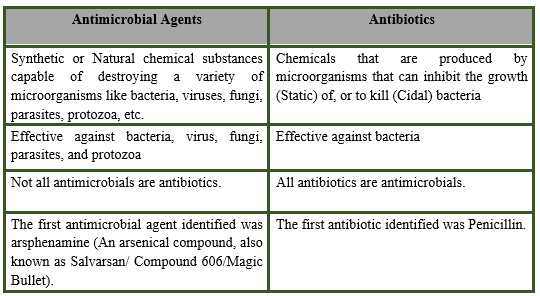
ANTIMICROBIAL AGENTS:
Antimicrobial agents are the substances produced by microorganisms having deleterious effects (static- stops the growth, cidal- killing) on other microbes in very low concentrations.
- It would be more meaningful to use the term antimicrobial agent (AMA) to designate synthetic as well as naturally obtained drugs that attenuate microorganisms, including Bacteria, Virus, Fungi, Parasites, Protozoa
ANTIMICROBIAL CLASSES:
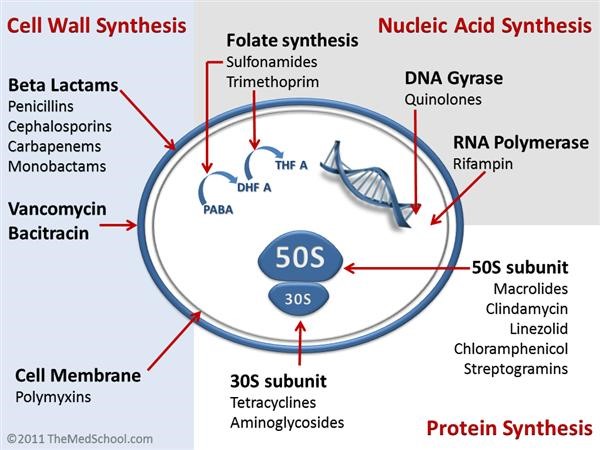
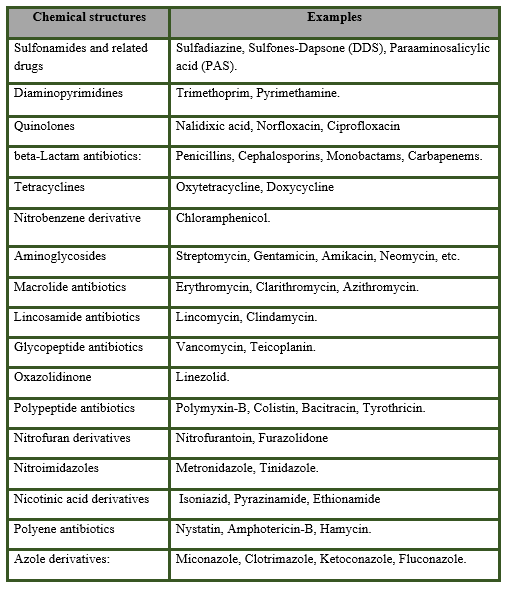
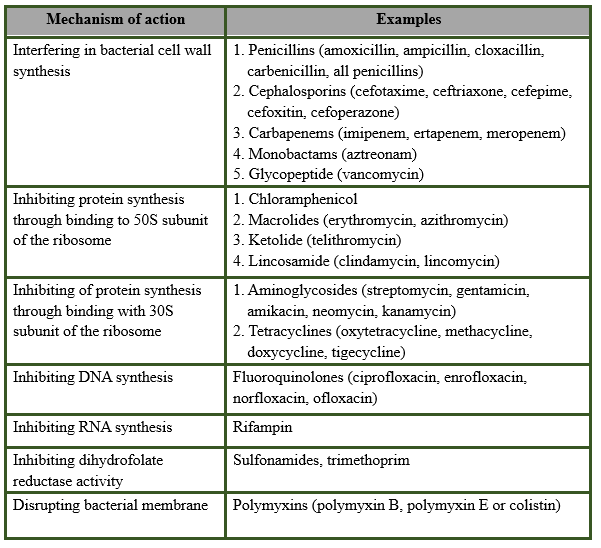
Antimicrobial agents include Antibiotics, Antiviral, Antifungal, Antiparasitic, and Antiprotozoal. Classification of antibiotics is based on their chemical structure (eg. ß-Lactam, Quinolones, Sulfonamide, etc) or based on their mechanism of action (e.g. cell wall synthesis inhibitor, protein synthesis inhibitors, DNA or RNA synthesis inhibitor, etc). Based on the action on bacteria, these agents are further classified into bactericidal and bacteriostatic. Bactericidal antibiotics are those that kill the bacteria; these agents are time or concentration-dependent. Time-dependent antibiotics (ß-lactam, Isoniazid, Rifampin, etc.) need a certain time of interaction of antibiotics on the bacteria to kill. Concentration-dependent antibiotics (Aminoglycoside, Bacitracin, and Quinolones) need a minimum concentration of the active agent at the target site to kill the organism. Bacteriostatic antibiotics are those antibiotics that inhibit the growth and multiplication of bacteria (e.g. Macrolides, Lyncosamide, and ß-Lactam).
Classification of Antimicrobial agents:
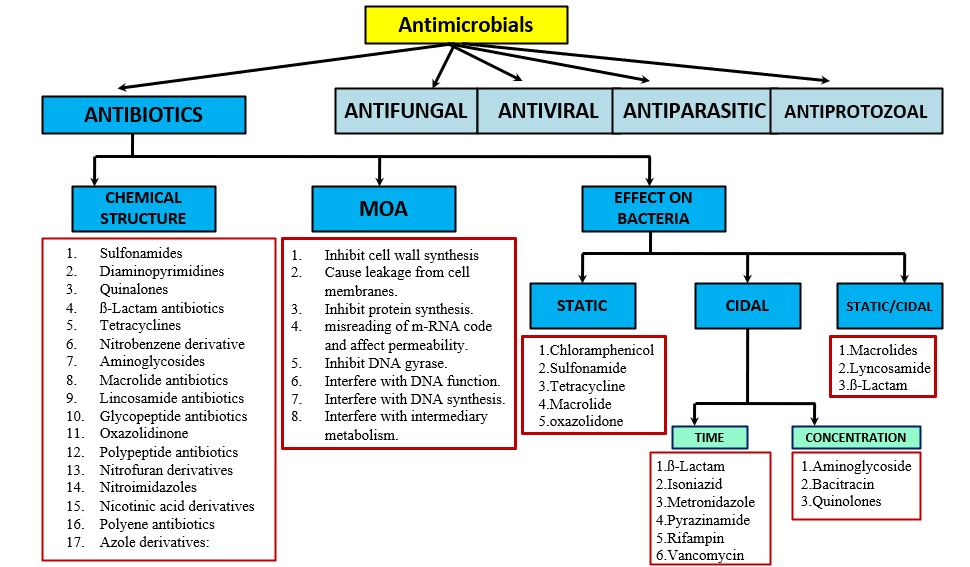
CLASSIFICATION BASED OF CHEMICAL STRUCTURES:
MECHANISM OF ACTION OF DIFFERENT ANTIBIOTIC CLASSES:
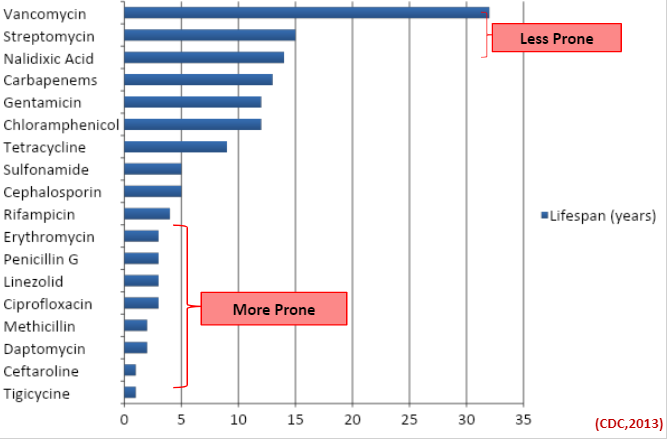
PRONENESS OF DIFFERENT CLASSES OF ANTIBIOTICS TO DEVELOPMENT OF RESISTANCE:
LIFESPAN OF DIFFERENT ANTIBIOTICS:
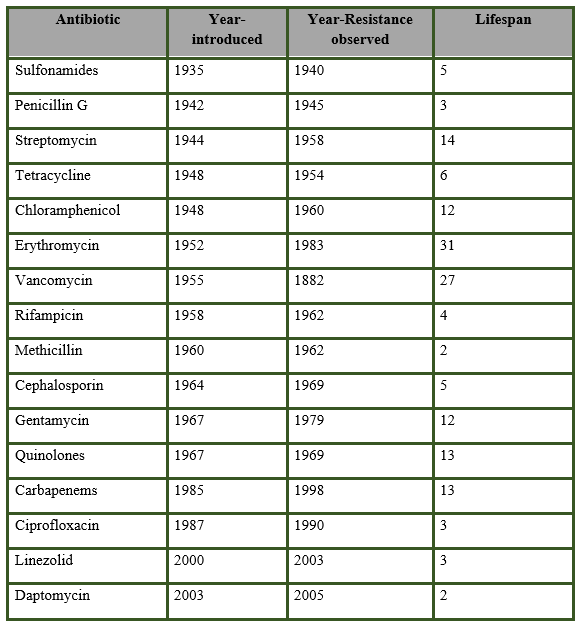
DIFFERENT CLASSES OF ANTIBIOTICS AND YEARS TAKEN TO DEVELOP RESISTANCE:
The proneness of different classes of antibiotics to the development of resistance is quite variable. Some groups are more prone to resistance and they took less time (< 3 years) to develop resistance like ß-Lactam, Tetracyclines, Macrolides, Quinolones, and some newer antibiotics (Synercid, Linezolid, Daptomycin). Aminoglycosides, Glycopeptides, Nalidixic acid, and Amino penicillin are less prone to resistance and they took more than 10 years to develop the first resistance in organisms.
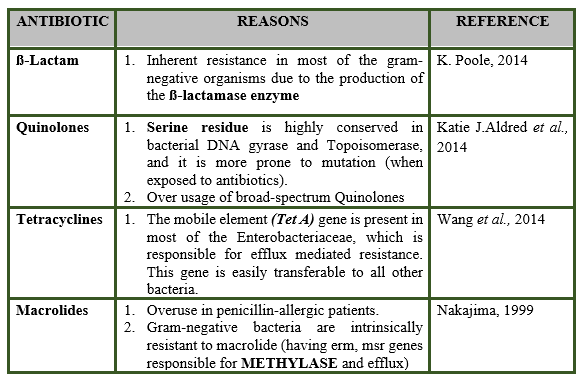
REASON FOR MORE PRONENESS:
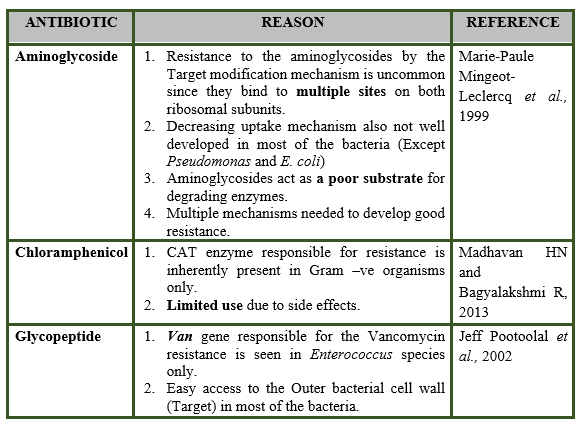
REASON FOR LESS PRONENESS:
References:
- Aldred, K.J., Kerns, R.J. and Osheroff, N., 2014. Mechanism of quinolone action and resistance. Biochemistry, 53(10), pp.1565-1574.
- Kumar, S. and Singh, B.R., 2013. An overview of mechanisms and emergence of antimicrobials drug resistance.
- Madhavan, H.N. and Bagyalakshmi, R., RESEARCH AND REVIEWS: JOURNAL OF MICROBIOLOGY AND BIOTECHNOLOGY.
- Mingeot-Leclercq, M.P., Glupczynski, Y. and Tulkens, P.M., 1999. Aminoglycosides: activity and resistance. Antimicrobial agents and chemotherapy, 43(4), pp.727-737.
Citation:
Nishanth Maria Anto Dani Nishanth, Palanichamy Pavithra – Different classes of Antimicrobial and their proneness to AMR. Resource page on Antimicrobial Resistance, The Vet Helpline E-magazine, Vol VIII (2020) ISSN 2454-9282 Available at: http://www.vethelplineindia.co.in/antimicrobial-resistance/